Brady: “Obamacare is imploding, and we’re just seeing prices skyrocket”
Our health care system continues to deteriorate under Obamacare. Americans are facing fewer choices, higher costs, and less access to the care they need. Just look at the news from last week:
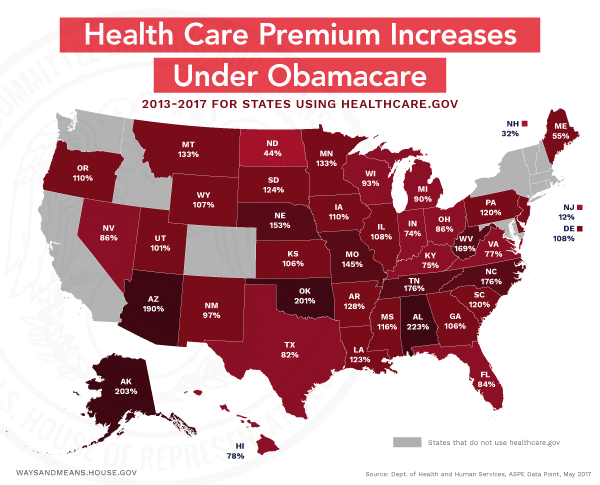
- Premiums have more than doubled under Obamacare. According to data from the previous Administration, millions of Americans are now paying twice as much—on average $3,000 more—for insurance on the individual marketplaces than they were in 2013.
- 25 more counties will have zero Obamacare insurance options. The last Obamacare insurer in parts of Missouri, Blue Cross Blue Shield of Kansas City, announced its decision to withdraw from Obamacare’s individual marketplace in 2018. That leaves hundreds of thousands more Americans with few, if any, places to turn for coverage.
Describing the urgent need to repeal and replace Obamacare, economist Stephen Moore wrote in The Washington Times:
“If we stay with Obamacare, within a few years tens of millions will have no insurance at all that is even remotely affordable. Aetna, Humana, and other major insurers in just recent months have fled Obamacare. The Titanic has hit the iceberg and it is rapidly sinking … Here’s a prediction: by the end of the year we could have nearly half the country without insurers if this spiral continues.”
House Republicans took action to rescue the American people from this failing law by passing the American Health Care Act, which the Congressional Budget Office confirmed:
- Lowers average premiums in the individual marketplace by 4 to 30 percent or more, depending on the state.
- Delivers nearly $1 trillion of relief from Obamacare taxes.
- Provides individuals and families freedom to choose a health care plan that is right for them.Obamacare keeps wreaking havoc across the country:
- Major insurers continue to abandon the individual insurance market in different states, making it more difficult for Americans to access coverage.
- Humana and Aetna announced they would withdraw from Obamacare’s individual exchanges entirely in 2018.
- The last remaining insurer in Iowa could exit the exchanges next year—leaving families in 94 out of 99 counties without a single insurer to turn to for their coverage.
- Connecticut, Maryland, New York, Oregon, and Virginia have already projected double-digit premium rate increases for next year.
As Ways and Means Republicans explain, Obamacare’s latest failures underscore the urgent need for the American Health Care Act—legislation passed by the House to fix our broken health care system:
On Delivering Relief from Obamacare
Rep. Diane Black (R-TN), Budget Committee Chairman, in RealClearPolitics: “Obamacare is a disaster, and in Tennessee, its collapse is creating dire circumstances for our citizens. Massive premium increases are making insurance unaffordable for more and more Tennesseans and rising deductibles are making it harder to get health care, even for those who have insurance. Doing nothing is not an option. Congress has taken the first step to keep our promise of repealing and replacing Obamacare.”
Rep. Kevin Brady (R-TX), Ways and Means Committee Chairman, in the Conroe Courier: “Although this is just the first step, it is a giant pivot in the right direction so that Americans no longer have to struggle under the $1 trillion in tax hikes brought on by Obamacare. Under the bill, Americans, especially small businesses, will no longer be forced to buy healthcare they do not want or cannot afford.”
Rep. Jackie Walorski (R-IN) in the South Bend Tribune: “Obamacare came with a lot of promises. But these promises were broken, and now many Hoosiers face higher premiums, fewer options, and a collapsing system … [AHCA] rescues Americans from the instability of Obamacare and begins a stable transition to a better system. It will lower premiums and strengthen markets so patients have real options they can actually afford. It will empower patients, not bureaucrats, to make health care decisions.”
On Protecting Patients with Pre-Existing Conditions
Rep. Erik Paulsen (R-MN) in the Minneapolis Star Tribune: “Nothing in this bill would allow an insurance company to deny someone coverage, including to those with a preexisting condition. Nothing would allow an insurance company to cancel someone’s insurance policy should they become sick. Despite claims from opponents, the bill does not classify sexual assault as a preexisting condition. For those who maintain continuous coverage, the bill does not allow insurance companies to charge an individual more simply because they have a preexisting condition. It’s also worth noting that this bill includes $138 billion to assist states in making sure everyone, including those with preexisting conditions, has access to high-quality, affordable health care.”
Rep. Adrian Smith (R-NE) in the Grand Island Independent: “I firmly believe we can protect access to care for those with preexisting conditions while lowering costs for the millions of Americans currently facing premiums and deductibles they cannot afford. Passing the American Health Care Act in the House was the first step, and we will continue our work in Congress to revive the health care marketplace.”
Rep. Jackie Walorski (R-IN) in the South Bend Tribune: “This bill maintains critical protections for patients with pre-existing conditions. I have always said any replacement must protect these patients, and we make sure no one can be denied coverage due to a pre-existing condition. States can obtain a waiver of some individual and small group insurance regulations to help lower premiums or increase the number of people with coverage, as long as they implement plans—such as high risk pools—to ensure affordable coverage for those with costly medical conditions. Under these waivers, insurers can only charge high-risk patients more if they have a two-month lapse in coverage, and the bill dedicates $8 billion to help patients in such situations.”
On Putting the American People Back in Control of Their Care
Rep. Carlos Curbelo (R-FL) in the Miami Herald: “I made a promise that I would fight for better healthcare for our country, for a market-based system where Americans, not special interests, are in control and can make the best healthcare choices for themselves and their families. The legislation before Congress today gets us closer to such a system.”
Rep. Erik Paulsen (R-MN) in the Minneapolis Star Tribune: “[This debate] is about Nyla, a recently widowed mother of four who saw her premiums jump to $1,000 per month with a $13,000 deductible… this debate is about Taryn, who, after being diagnosed with a brain tumor, suddenly had her plan canceled when her insurer pulled out of the market … [AHCA] is aimed at addressing many of the shortcomings of the ACA by stabilizing insurance markets and beginning to bring down premiums. Rather than the one-size-fits-all Washington approach, we can empower states and consumers to take control of their own health care outcomes.”
CLICK HERE to read Ways and Means Committee Chairman Brady’s statement on the AHCA.
CLICK HERE to read a summary of the AHCA.
CLICK HERE to read the section-by-section description of the AHCA.




 Back to the half a trillion dollars….
Back to the half a trillion dollars….