For many many months, the Trump administration was negotiating a peace deal with the Taliban. Frankly, all that the Taliban has agreed to, they have violated. Trump also issued a schedule to lower troop levels in Afghanistan to only a small tight residual number in May of 2021 along with contractors. With the new possible threat(s) of the Taliban and their growing connection to al Qaeda, Biden has decided to leave troop levels in the region at the present level with an increase in Syria and possibly Iraq. All the while, Iran just hosted a Taliban leader for talks where the topic(s) are unknown. Further, Taliban officials have been meeting in Moscow with Russian officials. Those details are found here.
President Biden also has another immediate issue before him and that is the release of a U.S. contractor that went missing in Afghanistan about a year ago. Mark Frerichs, a navy veteran went missing about a year ago while he was working as a contractor on an engineering project. It is thought he is in the custody of the Haqqani network. The U.S. State Department is offering a $5 million reward that leads to Frerichs’ return.
So, it is rather fitting that just this week, a very old FOIA request for former Defense Secretary Donald Rumsfeld documents have been released. Frankly, the questions which were referred to at the Pentagon as ‘snowflakes’ reflects his frustration of the layers of bureaucracy within the Department of Defense and his anger at getting real answers and challenging the quality of intelligence reports. Sound familiar? It is clearly a problem that after 20+ years has not found a quality solution. Just read a few of his snowflakes and judge for your self.
***
35 of the most notable items from the new collection is below from the National Archives.
A follow-on DNSA publication covering the rest of Rumsfeld’s tenure as secretary will appear through ProQuest later in 2021.
One such snowflake was written on March 3, 2003. At 8:16 AM, Rumsfeld wrote to Senior Military Assistant LTG Bantz J. Craddock and Department of Defense General Counsel William Haynes with the subject “KSM”. He wanted to know, “Do we know where the information to find Khalid Sheikh Mohammed came from? Was it from GTMO detainees?” There is no response from either Craddock or Haynes in the DOD release to the Archive, though Rumsfeld’s question is likely a push back to the false claims made by CIA Director George Tenet that the Agency’s resort to torture of Abu Zubaydah led to the capture of Khalid Sheikh Mohammed.
The Senate Select Committee on Intelligence torture report would later reveal that key intelligence on KSM as the mastermind of the 9/11 attacks came from the FBI’s non-coercive, rapport-building interrogation of Abu Zubaydah.[1] This success was prior to the CIA’s contract psychologists, James Mitchell and Bruce Jessen, taking over the interrogation at the CIA “Detention Site Green” in Thailand, which was created to house Zubaydah in 2002. Their approach to Zubaydah would include 83 water board sessions yet fail to produce any valuable intelligence. CIA clandestine services chief Jose Rodriguez (and perhaps Gina Haspel, who would later become DCI, though CIA redactions of documents continue to obscure her role) ordered the destruction of the torture videotapes, commenting that “the heat from destoying [sic] is nothing compared to what it would be if the tapes ever got into public domain.”
Later on March 3, under the subject “Contingencies”, Rumsfeld wrote to Under Secretary of Defense for Policy Doug Feith, stating, “We need to plan what we will do if Saddam Hussein is captured. We need to plan what we will do if we catch an imposter.” There is no record of Feith’s answer in the DOD release to the Archive.
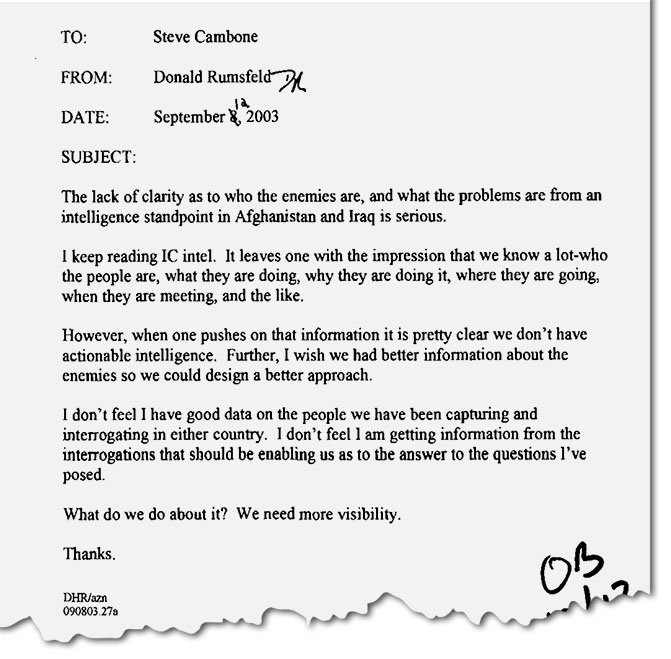
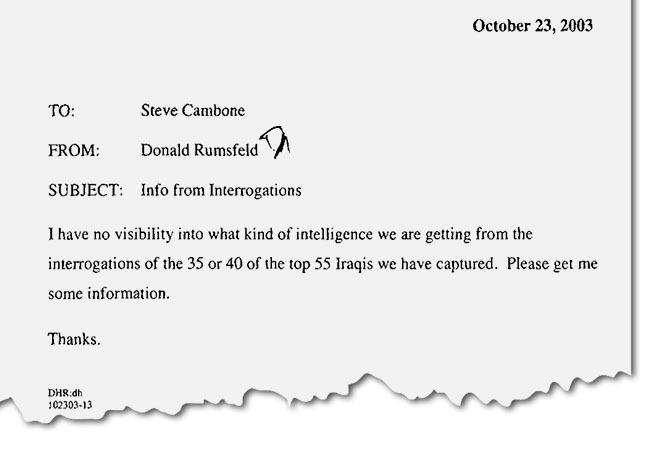
Throughout Rumsfeld’s tenure, his snowflakes circulated daily through the highest levels of the Pentagon. With scant limitations on their subject matter, the all-encompassing documents are sometimes an hourly paper trail inside the Office of the Secretary of Defense during six years of tremendous consequence for U.S. foreign policy. The declassified documents also provide an account that at times contradicts DOD public statements. For example, The Washington Post published a selection of the memos in the six part series “The Afghanistan Papers” in September 2019 revealing that officials misled the American public about the war in Afghanistan.
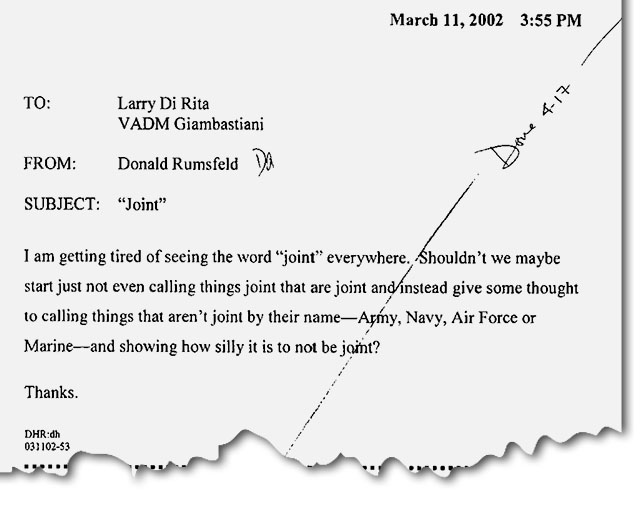
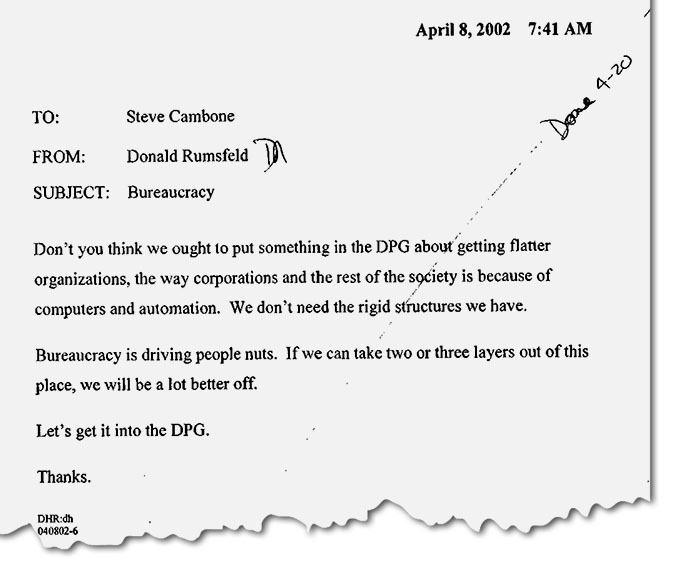
The entire corpus of snowflakes also details many aspects of the day-to-day operations of the Pentagon, the modernization of the U.S. armed forces, and Rumsfeld’s personal agenda against bureaucracy. “Bureaucracy is driving people nuts,” he wrote in an April 8, 2002, memo at 7:41AM. “If we can take two or three layers out of this place, we will be a lot better off.” In a separate April 8 letter, the secretary suggested cutting all major Pentagon programs by at least 20 percent. (The DOD budget increased by 37.54 percent between FY2001 and FY2006.) On March 11, 2002, Rumsfeld wrote to colleagues, “I am getting tired of seeing the word ‘joint’ everywhere.”

Other topics in the collection include:
- the military budgeting process and efforts to rein in defense spending;
- military planning, procurement, and expenditures;
- nuclear issues – weapons, proliferation, safety;
- decision making on military wages, benefits, tours of duty, and veterans issues;
- military intelligence;
- Defense Department relations with the CIA and Homeland Security;
- Rumsfeld’s relations with the State Department and National Security Council;
- U.S. relations with NATO;
- U.S. military relations with Russia, former Soviet republics, and other countries;
- Rumsfeld’s interactions with the news media, Congress, and the public;
- Guantanamo detainees, interrogation, and torture;
- concerns about the International Criminal Court and U.S. liability for war crimes;
- the hunt for Osama bin Laden and other terrorists;
- the Joint Strike Fighter program; and
- the emergency landing of a U.S. EP-3 at Hainan Island in 2001
Donald Rumsfeld’s Snowflakes, Part 1: The Pentagon and U.S. Foreign Policy, 2001-2003 will be a critical research tool for historians and will be available through many college and research libraries. Part II, which covers the last three years of Rumsfeld’s tenure as secretary of defense from 2004 to 2006, will be published in 2021. Learn more about accessing the Digital National Security Archive through your library online and how to request a free trial here.
A few more:
October 10, 2001
Rumsfeld requests a daily report on the location of Osama bin Laden.
November 8, 2001
Rumsfeld inquires: “Why doesn’t Pakistan sever its relationship with [sic] Taliban?”
November 29, 2001
Rumsfeld accuses career employees in the OSD of undermining his decisions and working too slowly.
February 15, 2002
Rumsfeld directs his staff to develop a white paper on detainees and the Geneva Conventions.
March 11, 2002
Rumsfeld suggests further classification review of the already pre-reviewed Annual Report to the President and the Congress.
March 11, 2002
Rumsfeld says the DOD annual report is not conclusive or upbeat enough.
March 12, 2002
Rumsfeld recounts his conversation with Russian MoD Sergei Ivanov at a Washington Wizards basketball game.
March 26, 2002
Under the subject “Business As Usual”, Rumsfeld questions whether the Department should cut educational programs while at war.
March 28, 2002
Rumsfeld pushes to lift restrictions on contractors providing force protection.
March 28, 2002
Rumsfeld proposes a weekly meeting on Afghanistan, stating that it is “drifting”.
April 8, 2002
Rumsfeld instructs his staff to create a list of all the major “processes” at the Pentagon and shorten them by atleast 20 percent.
April 9, 2002
Rumsfeld expresses concern about a “zero defect mentality” in promotion process.
April 12, 2002
Rumsfeld ruminates on the creation of a new Homeland Security Department.
April 15, 2002
Rumsfeld details a conversation with Henry Kissinger about the ICC.
April 23, 2002
Rumsfeld considers possibly renegotiating a Russia-NATO arrangement.
April 23, 2002
Rumsfeld proposes using contractors to train the Afghan army.
April 23, 2002
Rumsfeld asks if a DOD chart of the PPB system is a joke, or whether it should be.
May 5, 2002
Rumsfeld tells Hank Crumpton to “speak up”.
May 22, 2002
Rumsfeld circulates a letter comparing interrogation techniques in Afghanistan to Guantanamo.
August 8, 2002
Rumsfeld questions whether it is right for pilots to use amphetamines.
August 17, 2002
Rumsfeld ruminates on the U.S. and Western Europe “stopping proliferation, reducing weapons of mass destruction and contrubitng to peace and stability” around the world.
August 19, 2002
Rumsfeld addresses the President, Vice President, CIA Director, and National Security Advisor on U.S. policy towards Iran and North Korea.
October 1, 2002
Rumsfeld sends handwritten notes from an interview with a detainee to Fieth.
March 3, 2003
Rumsfeld requests a contingency plan for the possibility of capturing an imposter of Saddam Hussein.
March 3, 2003
Rumsfeld contacts Tenet about the intelligence that led to capturing KSM.
March 26, 2003
Rumsfeld requests material to brief the President privately on a post-Saddam Iraq.

%2FGettyImages-6596111491-5c2c1e0446e0fb0001254e42.jpg&f=1&nofb=1)



 It should also be noted that Anita Dunn was the top Biden campaign advisor.
It should also be noted that Anita Dunn was the top Biden campaign advisor.
